|
About the course:
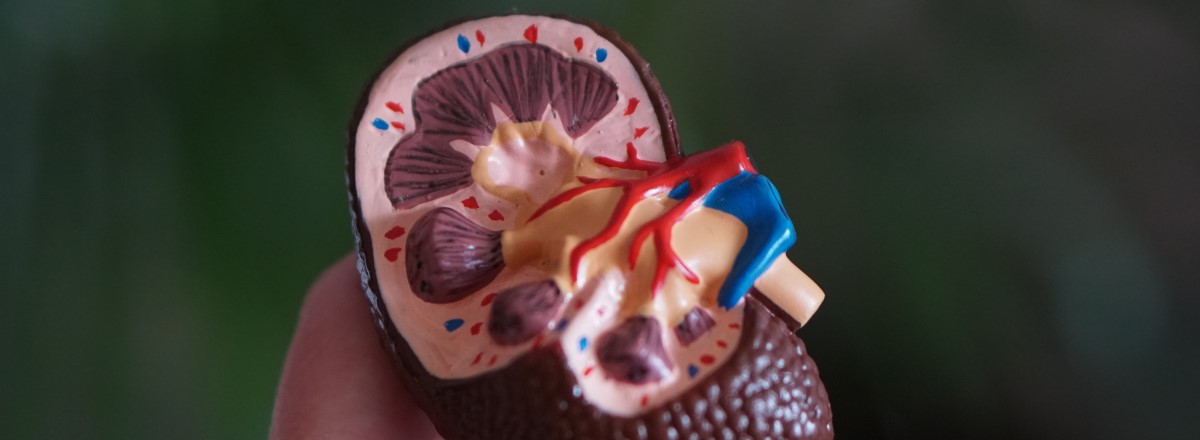
This course aims to prepare practitioners working in renal setting for their role within general nephrology and haemodialysis health care. They will have the opportunity to develop and critically evaluate specialist nephrology and haemodialysis skills and knowledge in order to deliver high quality and evidence based compassionate care. There will be emphasis on the wider context of care such as shared-decision making, social issues and the co-ordination of outside agencies.
At the end of the course you will be able to:
- Develop and critically review their own skills and competence in the holistic care of the patient within a renal care setting
- Enhance systematic assessment skills and professional experience in order to influence patient outcomes
- Select and critically evaluate relevant research in order to promote evidence-based practice within the renal care setting including national and international guidelines
- Synthesise knowledge and create responses to problems that expand / redefine existing practice in order to effect change within the practice setting
- Critically appraise and compare protocols and the management of care for patients with renal diseases clients locally, nationally and internationally in order to achieve clinical effectiveness
- Critically analyse the ethical, cultural, religious, spiritual and quality of life issues associated with renal disease, and debate how such issues are addressed in day-to-day practice
- Explain the different treatment options available and patient involvement in shared decision making demonstrating use of educational tools and an understanding of the patient pathway
- Critically evaluate and reflect on the professional role of the renal nurse within the inter-disciplinary settings and other members of the multi-disciplinary team to gain a more insightful perspective
- Critically examine strategies used for the assessment, management and evaluation of care to patients with acute and chronic renal disease to enhance clinical practice
- Critically discuss current resources in determining health care strategies for clients and their families / carers within the renal care setting
- Demonstrate academic reflection and reflective practice and the ability to audit own practice and make recommendations to achieve clinical effectiveness
Teaching arrangements
This module incorporates a blended learning approach, with 50% taught session and 50% E-learning. The educational approach is student centred and you will experience a wide variety of teaching and learning strategies, including:
- Lectures and discussions E-learning activities
- Worksheets
- Directed reading and study including online reading list
- Case studies and discussion
- Reflective practice
- Personal and group tutorials practice placements
The Assessment Portfolio
The assessment is a portfolio made up of 3 entries aiming to assess your knowledge and development. Your portfolio should demonstrate your achievement of the learning outcomes of the course.
All three portfolio entries (The e-learning quizzes, essay and e-PAD) must be submitted in order to pass the course.
Syllabus
Register your interest:
Please fill out the form below to register for the course. We will be in touch with further information.
About the author:
 |
Roseline Agyekum
FHEA MSc PG Cert HCP BSc CCN RN | Lecturer Practitioner | King's College Hospital NHS Foundation Trust
Roseline's educational research area is long term conditions with special interest in chronic kidney disease awareness especially among people of African and Afro-Caribbean Ancestry. Her publications have focused on vascular access longevity. Vascular access is the Achilles heel of haemodialysis as a renal replacement therapy.
Her role at King's College Hospital fosters the embedding of research into clinical care through Practice Development. She is involved in a number of Quality Improvement projects to deliver harm-free evidence based care to patients. She is intentional about developing an empowered, motivated, and sustainable renal workforce.
|
Course design:
 |
Florin Ivan
Project Manager, Learning Hub | King's Health Partners
|
|